The CoVID-19 Immune Paradox
During the pandemic, the primary focus has been on boosting and maintaining high COVID-19 antibody levels (the adaptive immune response). However, this approach has had unintended consequences.
By emphasizing antibodies, less attention has been given to the innate immune response, our first line of defense against infection - which plays a crucial role in resisting novel pathogens and emerging variants.
An immune paradox
Lack of Innate Immune Training
While effective against specific pathogens, a strong adaptive immune response can reduce innate immune training by bypassing or shortening the innate systems engagement with a pathogen. That is, when the adaptive immune system quickly produces antibodies and T-cell responses against a specific pathogen, it can neutralize the infection before the innate immune cells have enough time to undergo sufficient training or reprogramming.
This reduces the innate systems exposure to the pathogen, limiting its ability to develop a broader, more generalized response in tackling future novel pathogens or emerging variants.
In contrast, repeated natural exposure to infections can strengthen innate immune memory, a process known as trained immunity, which helps the body respond more effectively to diverse threats.
Immune Imprinting
Furthermore, in the context of CoVID-19, both vaccination and severe infection can program the adaptive immune system to hyper-focus its response on the original Wuhan strain, even when encountering new variants. This well-known phenomenon is called immune imprinting.
The results below show that after a booster for a new COVID strain, the antibody response remained overwhelmingly directed at the original Wuhan strain, with minimal response to the booster strain (antibody titers: 25,954 against the original strain vs. antibody titer: 59 against the booster strain used).
Source: N. Lasrado et al. Antibodies directed at Wuhan strain 25,954 compared to 59 directed at XBB.1.6 three weeks after bivalent booster. Month 3: 21,804 against wuhan strain and 70 against XBB.1.6
If a single stable COVID-19 strain had persisted, immune imprinting would have been strongly protective and not an issue as with other vaccines like measles for example. However, the rapid emergence of new covid variants has made the imprinted antibody response less effective, leading to incomplete viral neutralization. Additionally, a mismatched (suboptimal) antibody response can still suppress innate immunity, further hindering its ability to adapt to evolving variants.
Unless severe, infection prior to initial vaccination may help reduce immune imprinting by training the innate immune system through natural exposure.
Antibody Dependent Enhancement of Infection
Another concern is antibody-dependent enhancement of infection (ADEI), seen after vaccination for dengue and other coronaviruses, where high titers of antibodies facilitate viral entry into cells instead of neutralizing the virus.
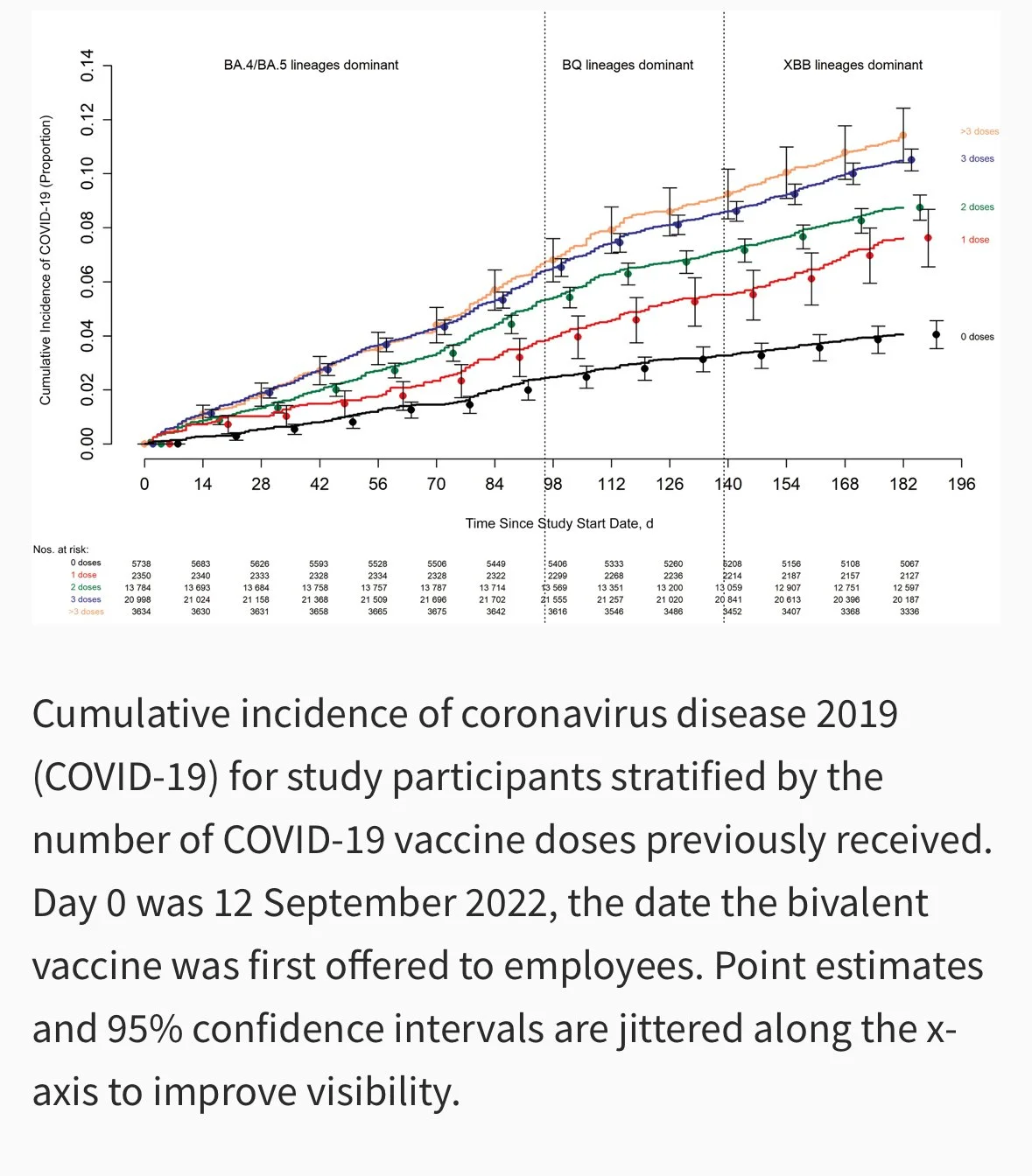
The combined effects of poor innate immune training, immune imprinting, and ADEI may help explain the Cleveland Clinic study by Shrestha et al., which found a strong correlation between increasing vaccine doses and higher COVID-19 infection rates.
Source Shresthra et al
Boost Your Innate Immunity
The good news is that it is possible to boost your innate immune function by various lifestyle approaches and specific evidence based medical interventions. The interventions recommended by Luminnova Health are outlined in this article. Boosting innate immunity is the foundation but there are a number of additional measures that can be taken to lessen the risk of infection or respond rapidly if symptoms develop. These are covered in our Viral Defense Strategies article.